Plexiform Lesions in Pulmonary Hypertension – Unraveling a Key Pathology
Introduction
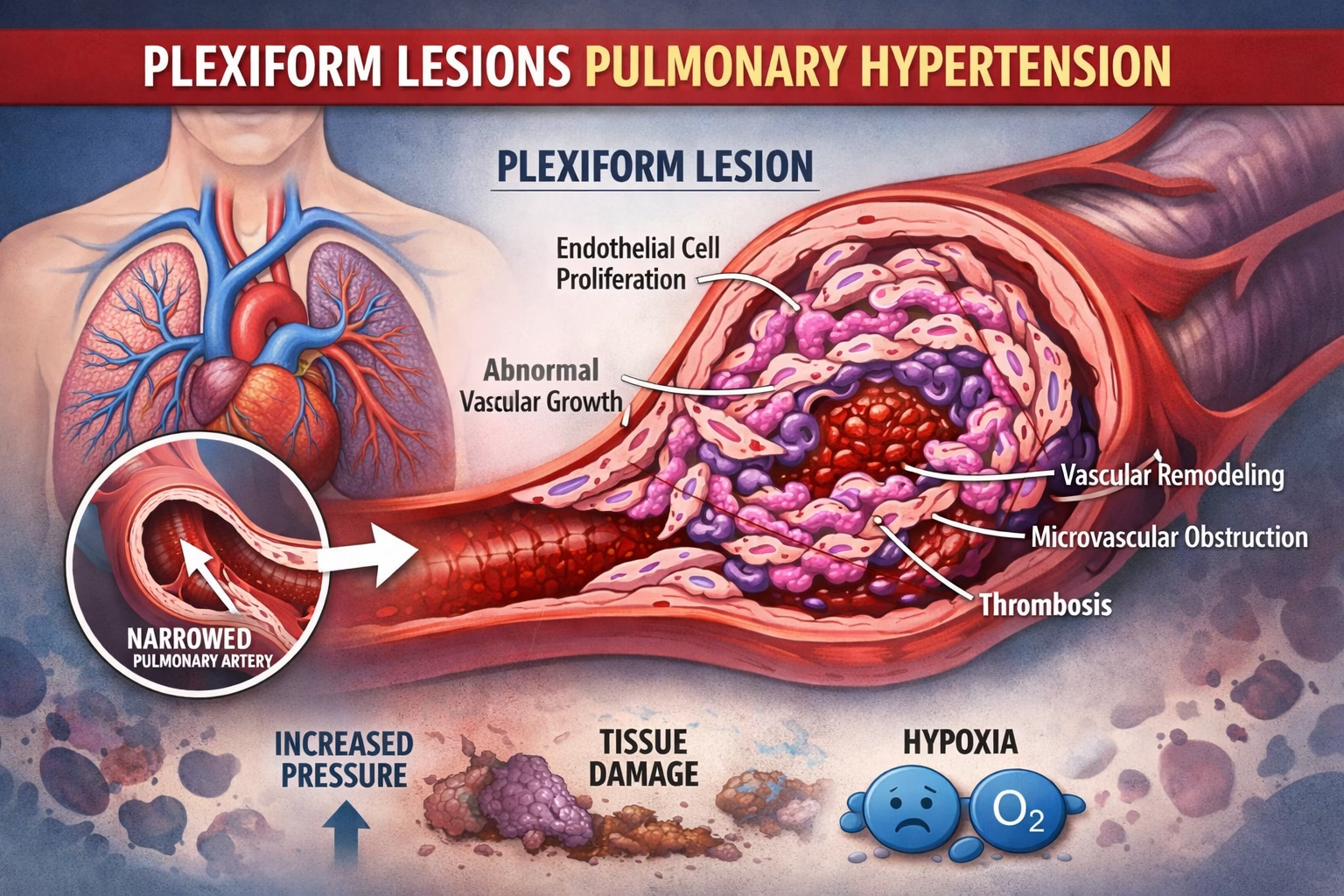
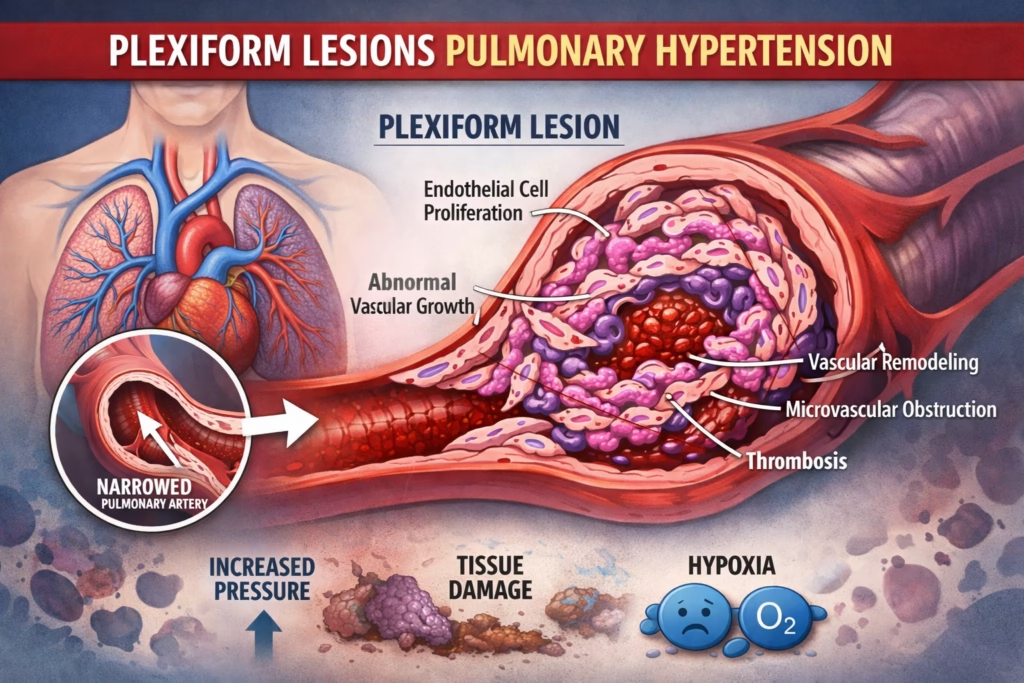
Pulmonary hypertension (PH) is a complex, progressive disease defined by elevated pressure in the pulmonary arteries, which can lead to right heart strain and ultimately heart failure if untreated. Among the multiple vascular changes observed in PH, plexiform lesions stand out as a hallmark of advanced and severe disease.
These lesions are not merely microscopic curiosities, they represent profound structural changes that disrupt normal blood flow and indicate irreversible remodeling of the pulmonary vasculature. In this post, we’ll explore:
-
What plexiform lesions are
-
How they develop
-
Their clinical significance
-
How they are diagnosed
-
Implications for treatment and prognosis
-
Emerging research targeting their underlying mechanisms
This guide is aimed at clinicians, researchers, and anyone seeking a deeper understanding of pulmonary hypertension pathology.
Section 1: What Are Plexiform Lesions?
Plexiform lesions are complex, tangled networks of proliferating endothelial and smooth muscle cells within the small arteries of the lungs. These lesions are most commonly found in small pulmonary arteries (<500 µm in diameter), often at branch points, where turbulent blood flow may exacerbate injury.
Key features of plexiform lesions:
-
Endothelial and smooth muscle proliferation: Excess growth leads to abnormal vessel architecture.
-
Interconnected vascular channels: The vessels form multiple small, web-like lumens instead of a single clear channel.
-
Obliterated lumen: The original vessel is partially or completely blocked, increasing resistance to blood flow.
-
Branch-point predilection: They tend to form where blood vessels split, a location susceptible to mechanical stress and turbulent flow.
Think of plexiform lesions as “knots” in the pulmonary arteries, they reduce effective blood flow, raise vascular resistance, and place increased strain on the right ventricle.
Section 2: The Pathophysiology Behind Plexiform Lesions
1. Endothelial Dysfunction
-
Triggered by genetic predisposition (e.g., BMPR2 mutations), chronic inflammation, or environmental toxins.
-
Leads to an imbalance in vasoactive mediators:
-
Decreased vasodilators (nitric oxide, prostacyclin)
-
Increased vasoconstrictors (endothelin-1)
-
-
This imbalance sets the stage for uncontrolled vascular remodeling.
2. Abnormal Cell Proliferation
-
Endothelial cells, smooth muscle cells, and fibroblasts proliferate excessively.
-
Neointimal formations (“mulberry-like” clusters) evolve into the web-like plexiform structures.
-
These structures can recruit inflammatory cells and secrete growth factors, further exacerbating vascular remodeling.
3. Vascular Remodeling and Increased Resistance
-
Thickening of the vessel wall and luminal narrowing increase pulmonary vascular resistance.
-
Elevated resistance imposes chronic afterload on the right ventricle, leading to right heart hypertrophy, dysfunction, and eventually failure.
In essence, plexiform lesions are both a marker and a driver of disease progression in pulmonary hypertension.
Section 3: Clinical Significance in Pulmonary Hypertension
Plexiform lesions are most commonly associated with:
-
Idiopathic Pulmonary Arterial Hypertension (IPAH)
-
Heritable Pulmonary Arterial Hypertension
-
Certain connective tissue disease–associated PH (e.g., systemic sclerosis)
Why plexiform lesions matter:
-
They correlate strongly with disease severity and poor prognosis.
-
Indicate irreversible vascular remodeling, meaning some damage cannot be reversed with vasodilator therapy.
-
Patients with plexiform lesions often show limited response to standard treatments, emphasizing the need for early diagnosis and intervention.
Section 4: Diagnosing Plexiform Lesions
Diagnosing plexiform lesions during life is challenging, as definitive identification requires histology. However, clinicians use a combination of indirect and direct methods:
1. Right Heart Catheterization
-
Gold standard for measuring pulmonary artery pressures.
-
Confirms pulmonary arterial hypertension (PAH) and helps classify subtypes.
2. Imaging Techniques
-
High-Resolution CT (HRCT): May show mosaic perfusion patterns, central artery enlargement, or subtle vessel pruning.
-
Emerging molecular imaging: PET tracers targeting endothelial proliferation or vascular remodeling are being investigated for earlier detection.
3. Tissue Biopsy (Rarely Performed)
-
Transbronchial or open lung biopsy can reveal classic plexiform structures.
-
Reserved for atypical or research cases due to risk of complications such as bleeding.
Section 5: Treatment Implications
Currently, there are no therapies that directly reverse plexiform lesions, but understanding their presence influences treatment strategy:
Medical Management Goals
-
Reduce pulmonary vascular resistance
-
Improve right ventricular function
-
Delay or prevent further vascular remodeling
Common drug classes:
-
Endothelin receptor antagonists (ERAs): e.g., bosentan, ambrisentan
-
Phosphodiesterase-5 inhibitors (PDE5i): e.g., sildenafil, tadalafil
-
Prostacyclin analogs/receptor agonists: e.g., epoprostenol, selexipag
Advanced interventions:
-
Atrial septostomy: Palliative shunt to unload the right heart in severe cases
-
Lung transplantation: Definitive treatment for eligible patients with advanced, irreversible disease
Section 6: Research and Future Directions
Innovative research aims to prevent or reverse plexiform lesion formation:
Targeting Growth Factor Pathways
-
Inhibitors of PDGF, TGF-β, VEGF may reduce abnormal vascular proliferation.
Gene and Cell Therapy
-
Gene editing for BMPR2 mutations
-
Endothelial progenitor cell therapy to restore healthy vascular lining
Novel Imaging Biomarkers
-
Molecular probes for early detection of active vascular remodeling
-
Could allow intervention before lesions become irreversibly established
Conclusion
Plexiform lesions are not just microscopic curiosities, they are central to the pathophysiology and progression of advanced pulmonary hypertension. These tangled webs of proliferating cells obstruct blood flow, contribute to right heart strain, and signal irreversible vascular remodeling, often correlating with poor prognosis.
While current therapies focus on symptom management and vasodilation, the ultimate goal is to prevent lesion formation or reverse existing lesions. Cutting-edge research into growth factor inhibition, gene therapy, and regenerative medicine holds promise for more effective, targeted treatments in the future.
Understanding plexiform lesions allows clinicians, researchers, and patients to appreciate the urgency of early diagnosis, tailored therapy, and continued innovation in the battle against pulmonary hypertension.