Introduction
Hypertension, often dubbed the “silent killer,” affects nearly one-third of adults worldwide. Because symptoms can be subtle or absent, many people remain unaware of their high blood pressure until complications arise. For nurses on the front lines of patient care, early identification and management of hypertension are critical. One of the most powerful tools in a nurse’s toolkit is the nursing diagnosis—a clinical judgment that identifies patient problems and guides evidence-based interventions. In this blog post, we’ll explore the role of nursing diagnosis in hypertension management, identify common diagnoses, outline targeted interventions, and highlight strategies for patient education and follow-up. Whether you’re a nursing student or a seasoned clinician, this guide will help you refine your approach to caring for patients with elevated blood pressure.

Understanding Hypertension
Defining Hypertension
• Primary (essential) hypertension: No identifiable cause; accounts for 90–95% of cases.
• Secondary hypertension: Caused by an underlying condition (e.g., renal disease, endocrine disorders).
Risk Factors
• Nonmodifiable: Age, family history, ethnicity
• Modifiable: Diet (high salt intake), obesity, physical inactivity, stress, tobacco/alcohol use
Complications of Uncontrolled Hypertension
• Cardiovascular: Heart failure, myocardial infarction, stroke
• Renal: Chronic kidney disease
• Neurological: Cognitive decline, vision impairment
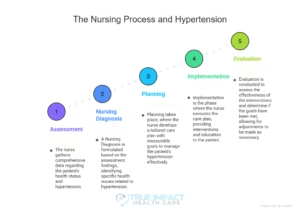
The Nursing Process and Hypertension
The nursing process assessment, diagnosis, planning, implementation, and evaluation—is the framework for delivering individualized nursing care. In hypertension management, a thorough assessment sets the stage for accurate diagnosis and effective interventions.
- Assessment
– Vital signs: Multiple accurate blood pressure readings (sitting, standing, both arms)
– Health history: Duration of hypertension, medication adherence, comorbidities
– Lifestyle factors: Diet, exercise, stress levels, substance use
– Physical exam: Signs of target organ damage (e.g., heart sounds, retinal changes, peripheral pulses)
– Lab data: Lipid profile, electrolytes, renal function tests, ECG changes - Nursing Diagnosis
Based on the assessment data, nurses formulate diagnoses that pinpoint patient needs. Common nursing diagnoses for hypertension include:
• Ineffective Health Management related to lack of knowledge or poor adherence to treatment regimen
• Knowledge Deficit (Disease Process, Medication Regimen, Dietary Modifications)
• Anxiety related to fear of complications or lifestyle changes
• Risk for Ineffective Tissue Perfusion (Renal, Cerebral, Cardiopulmonary)
• Risk for Imbalanced Nutrition: More Than Body Requirements
• Activity Intolerance related to fatigue or cardiovascular limitations
- Planning
For each diagnosis, nurses develop SMART goals (Specific, Measurable, Achievable, Realistic, Time-bound). Example: “Patient will demonstrate correct self-monitoring of blood pressure and record readings twice daily by discharge.” - Implementation
Nursing interventions target both physiologic and psychosocial aspects of hypertension. See the next section for detailed strategies. - Evaluation
Nurses continually assess progress toward goals. If targets aren’t met, the care plan is revised to address barriers.
Common Nursing Diagnoses and Interventions for Hypertension
- Ineffective Health Management
Definition: Inability to manage health regimen
Key Assessment Cues: Missed medications, poor follow-up appointment attendance, inconsistent blood pressure monitoring
Interventions:
• Educate patient on the importance of medication adherence and the risks of uncontrolled hypertension.
• Collaborate with the healthcare team to simplify drug regimens (e.g., once-daily dosing, combination pills).
• Arrange for home health visits or telehealth monitoring to reinforce self-care behaviors.
Expected Outcomes:
– Patient will verbalize understanding of medication schedule and treatment goals.
– Patient will maintain blood pressure within target range (e.g., <130/80 mmHg). - Knowledge Deficit
Definition: Lack of cognitive information about disease, treatment, or procedures
Key Assessment Cues: Patient statements of confusion, incorrect self-care behaviors
Interventions:
• Provide one-on-one teaching using plain language and visual aids.
• Demonstrate blood pressure monitoring technique; have patient return demonstration.
• Supply written materials and reputable online resources.
Expected Outcomes:
– Patient will describe at least three lifestyle modifications to control blood pressure.
– Patient will accurately record and interpret blood pressure readings. - Anxiety
Definition: Vague apprehension related to health status and lifestyle modifications
Key Assessment Cues: Restlessness, sleep disturbances, voiced fears about complications
Interventions:
• Offer emotional support; encourage patient to verbalize concerns.
• Teach relaxation techniques (deep breathing, guided imagery).
• Involve family members in education to build a support system.
Expected Outcomes:
– Patient will report reduced anxiety levels (e.g., using a 0–10 anxiety scale).
– Patient will demonstrate at least one relaxation technique during stressful situations. - Risk for Ineffective Tissue Perfusion
Definition: Vulnerable to decreased blood flow to organs
Key Assessment Cues: History of end-organ damage, elevated readings despite treatment
Interventions:
• Monitor vital signs and neurological status at prescribed intervals.
• Administer antihypertensive medications as ordered; observe for side effects (e.g., orthostatic hypotension).
• Encourage gradual position changes to prevent dizziness.
Expected Outcomes:
– Patient will maintain adequate perfusion (e.g., warm extremities, capillary refill <3 seconds).
– No signs of end-organ damage (e.g., stable creatinine, clear neurological exam).
Patient Education Strategies
Effective patient education is the cornerstone of long-term hypertension control. Consider the following tips:
• Use the teach-back method to confirm understanding.
• Customize dietary advice (e.g., DASH diet, salt substitutes) to cultural preferences.
• Set incremental goals (e.g., reduce sodium intake by 500 mg per week).
• Encourage regular physical activity: start with 10–15 minute walks and build up.
• Discuss stress management: mindfulness, yoga, social support networks.
• Provide resources: community support groups, smartphone apps for tracking blood pressure and medication reminders.
Documentation and Continuity of Care
Accurate nursing documentation ensures continuity across shifts and disciplines. Include:
• Baseline and ongoing blood pressure readings
• Patient’s self-monitoring logs
• Education topics covered and patient responses
• Behavioral changes and barriers identified
• Revisions to the care plan based on evaluation
Coordinate with dietitians, pharmacists, social workers, and primary providers to create a cohesive plan that addresses all facets of the patient’s condition from medication affordability to psychosocial stressors.
Conclusion
Hypertension remains a leading contributor to cardiovascular morbidity and mortality, but timely nursing diagnosis and targeted interventions can significantly improve patient outcomes. By systematically assessing risk factors, formulating accurate nursing diagnoses, and deploying individualized care plans, nurses empower patients to take charge of their health. Remember that education, empathy, and collaboration are just as vital as clinical expertise. As healthcare providers, our goal is not only to lower numbers on a blood pressure cuff but also to foster sustainable lifestyle changes that enhance quality of life. Armed with the strategies outlined here, you’re well equipped to make a meaningful impact in the lives of patients living with hypertension.











One Response