Introduction
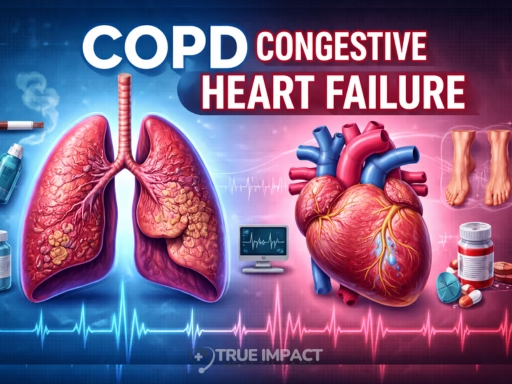
It’s common for people to confuse medical conditions that share overlapping symptoms. One question frequently raised is: “Is COPD the same as congestive heart failure?”
Both conditions can lead to shortness of breath, fatigue, and reduced tolerance for physical activity, symptoms that understandably blur the distinction. However, they arise from fundamentally different physiological problems. COPD primarily affects the lungs and airflow, whereas congestive heart failure (CHF) stems from impaired cardiac pumping and circulatory dynamics.
Understanding the difference is more than academic, it directly impacts treatment choices, long-term management, and patient outcomes. This article breaks down what each condition involves, explores why they can appear similar, explains how clinicians differentiate between them, and outlines practical approaches to treatment and lifestyle management.
Understanding COPD
What Is COPD?
Chronic Obstructive Pulmonary Disease (COPD) refers to a group of progressive lung disorders — most commonly emphysema and chronic bronchitis — that cause persistent airflow limitation.
-
Emphysema destroys alveoli (air sacs), reducing gas exchange surface area
-
Chronic bronchitis causes airway inflammation and mucus overproduction
The resulting airflow obstruction is typically irreversible and worsens gradually over time.
Pathophysiology in Brief
COPD alters lung mechanics in several ways:
-
Narrowed airways increase resistance during exhalation
-
Loss of elastic recoil traps air in the lungs
-
Impaired oxygen exchange reduces blood oxygen levels
This leads to the hallmark sensation of air hunger and progressive respiratory compromise.
Key Features of COPD
Common clinical characteristics include:
-
Progressive breathlessness (initially during exertion)
-
Chronic productive cough
-
Wheezing or chest tightness
-
Frequent respiratory infections
-
Reduced exercise tolerance
Symptoms often develop slowly, which can delay diagnosis.
Risk Factors
Major contributors include:
-
Long-term cigarette smoking
-
Exposure to air pollution or industrial irritants
-
Biomass fuel exposure (in poorly ventilated settings)
-
Genetic predisposition such as alpha-1 antitrypsin deficiency
Smoking cessation remains the single most impactful preventive measure.
Understanding Congestive Heart Failure
What Is Congestive Heart Failure?
Congestive heart failure is a syndrome in which the heart cannot pump sufficient blood to meet the body’s needs.
Two principal mechanisms exist:
-
Systolic dysfunction — weakened contraction reduces ejection of blood
-
Diastolic dysfunction — stiff heart muscle impairs filling
Fluid accumulation occurs when circulation backs up, leading to congestion in lungs and tissues.
Physiological Mechanisms
In CHF:
-
Reduced cardiac output activates compensatory hormonal pathways
-
Sodium and water retention increase blood volume
-
Fluid accumulates in lungs or peripheral tissues
These processes create the characteristic swelling and respiratory symptoms.
Key Features of CHF
Typical symptoms include:
-
Breathlessness when lying flat (orthopnea)
-
Swelling in lower limbs or abdomen
-
Persistent cough or wheezing
-
Extreme fatigue
-
Irregular or rapid heartbeat
Advanced cases may produce frothy sputum due to pulmonary fluid buildup.
Risk Factors
CHF often arises from underlying cardiovascular disease:
-
Coronary artery disease
-
Hypertension
-
Diabetes
-
Prior heart attack
-
Valve disorders
These factors weaken cardiac structure or function over time.
Why the Confusion? Overlapping Symptoms
COPD and CHF share several outward manifestations:
-
Shortness of breath
-
Exercise intolerance
-
Chronic coughing
-
Sleep disturbances
The overlap occurs because both impair oxygen delivery, albeit through different mechanisms (ventilation vs circulation). This similarity underscores the importance of thorough evaluation rather than symptom-based assumptions.
Distinguishing COPD from CHF
Accurate diagnosis requires combining clinical insight with diagnostic testing.
Patient History and Physical Exam
Clues that guide differentiation:
-
Smoking or pollutant exposure → suggests COPD
-
Cardiac disease or fluid retention → suggests CHF
-
Wheezing or prolonged exhalation → favors COPD
-
Jugular vein distension or heart sounds → favors CHF
No single sign is definitive; interpretation depends on pattern recognition.
Diagnostic Tests
Physicians rely on objective tools:
-
Spirometry — confirms airflow obstruction
-
Imaging (X-ray/CT) — lung hyperinflation vs cardiac enlargement
-
Echocardiography — evaluates pumping efficiency
-
BNP blood test — elevated in heart failure
Combined testing provides diagnostic clarity.
Response to Treatment
Therapeutic response can also offer insight:
-
Improvement with bronchodilators → COPD
-
Improvement with diuretics → CHF
This is often used alongside diagnostic evidence.
When Both Conditions Coexist
Comorbidity is common, particularly in aging populations.
Management considerations include:
-
Coordinated pulmonary and cardiac therapy
-
Careful fluid management
-
Monitoring kidney function and electrolytes
-
Lifestyle adjustments (smoking cessation, diet, exercise)
Multidisciplinary care significantly improves outcomes.
Treatment and Management Strategies
COPD Treatment Highlights
-
Bronchodilators to improve airflow
-
Inhaled corticosteroids for exacerbation control
-
Pulmonary rehabilitation programs
-
Supplemental oxygen when needed
Long-term management emphasizes lung preservation and symptom control.
CHF Treatment Highlights
-
Diuretics to reduce fluid overload
-
ACE inhibitors or ARBs for cardiac support
-
Beta blockers for workload reduction
-
Sodium restriction and fluid management
Care focuses on optimizing cardiac function and preventing progression.
Broader Lifestyle Considerations
Regardless of diagnosis:
-
Maintain physical activity within tolerance
-
Follow dietary guidance
-
Monitor symptoms regularly
-
Adhere strictly to medications
-
Attend routine follow-ups
Patient engagement strongly influences long-term stability.
Conclusion
Although COPD and congestive heart failure can present with similar outward symptoms, they originate from distinct physiological dysfunctions, pulmonary airflow limitation versus cardiac pumping failure. Accurate differentiation relies on comprehensive clinical evaluation and targeted diagnostic testing.
Recognizing the difference ensures appropriate treatment, prevents complications, and supports better quality of life. Anyone experiencing persistent breathlessness, swelling, or chronic coughing should seek medical assessment promptly, early identification remains one of the most powerful tools in managing chronic disease effectively.











One Response