Is Congestive Heart Failure Reversible? Understanding Your Options and Outlook
Introduction
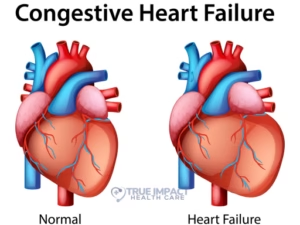
Few diagnoses strike more fear into patients and families than congestive heart failure (CHF). When the heart can’t pump blood efficiently, fluid builds up in the lungs and body, leaving you breathless, fatigued, and anxious about the future. But here’s the hopeful question on everyone’s mind: Is congestive heart failure reversible? In this post, we’ll explore what “reversible” really means, which factors play a role, and the treatments and lifestyle changes that can help your heart recover as much function as possible.
What Is Congestive Heart Failure?
Before discussing reversibility, let’s cover the basics. Congestive heart failure is not a single disease but a syndrome in which the heart’s pumping capacity is impaired. Key points include:
• HFpEF vs. HFrEF: Preserved ejection fraction (HFpEF) means the heart contracts normally but can’t fill properly; reduced ejection fraction (HFrEF) means the heart’s contraction is weakened.
• Left-sided vs. right-sided: Left-sided failure often causes pulmonary congestion (fluid in the lungs); right-sided failure leads to fluid accumulation in the legs, abdomen, and liver.
• Stages A–D: The American College of Cardiology/American Heart Association stages range from “at risk” (A) to “advanced” (D).
Common Causes and Risk Factors
Several conditions and lifestyle factors can trigger or worsen CHF:
• Coronary artery disease and heart attacks
• High blood pressure (hypertension)
• Diabetes and metabolic syndrome
• Obesity and sedentary lifestyle
• Valvular heart disease
• Myocarditis and other infections
• Toxins (e.g., alcohol, certain chemotherapy agents)

What Does “Reversible” Actually Mean?
In the context of CHF, “reversible” refers to measurable improvement in heart structure and function, sometimes called “reverse remodeling.” Full normalization of function is rare in chronic irreversible damage, but significant improvement can be achieved, especially if:
• The underlying cause is addressed (e.g., treating thyroid disease or removing a toxin).
• Therapy is initiated early in the disease process.
• Patients adhere strictly to medications and lifestyle changes.
Evidence-Based Treatments That Promote Reversal
Modern heart-failure therapies can improve symptoms, reduce hospitalizations, and in many cases partially restore heart function. Key strategies include:
- Medications
• ACE inhibitors or ARBs: Reduce workload on the heart and prevent remodeling
• Beta-blockers: Slow heart rate, improve efficiency, and protect against stress hormones
• Mineralocorticoid receptor antagonists (spironolactone, eplerenone)
• SGLT2 inhibitors (e.g., dapagliflozin): Originally for diabetes but now a cornerstone in HFrEF care
• Diuretics: Relieve fluid overload and improve breathing - Device-Based Therapies
• Cardiac resynchronization therapy (CRT): Coordinates heart’s contractions in select HFrEF patients
• Implantable cardioverter-defibrillators (ICDs): Prevent sudden cardiac death
• Left ventricular assist devices (LVADs): Mechanical pump support for advanced stages - Lifestyle Modifications
• Low-sodium, heart-healthy diet (DASH-style)
• Regular, tailored exercise program (often under cardiac rehabilitation)
• Weight management and fluid monitoring (daily weight checks)
• Smoking cessation and alcohol moderation
• Stress reduction (mindfulness, counseling) - Addressing Underlying Causes
• Revascularization for coronary artery disease (angioplasty or bypass surgery)
• Valve repair or replacement for severe valvular disease
• Treatment of arrhythmias (e.g., atrial fibrillation ablation)
• Management of endocrine disorders (thyroid, diabetes)
Factors That Influence Recovery
Not every patient responds the same. Predictors of a better chance at reversal include:
• Earlier stage at diagnosis
• Non-ischemic causes (for example, viral myocarditis can heal)
• Good adherence to medical and lifestyle regimens
• Younger age and fewer comorbidities
• Access to specialized heart-failure centers
When Full Reversal Isn’t Possible
In many chronic cases, complete normalization of heart function remains out of reach. Yet even partial improvement can translate into:
• Improved quality of life
• Fewer hospital visits
• Increased exercise tolerance
• Prolonged survival
Management then focuses on symptom relief, preventing progression, and maintaining day-to-day function.
The Importance of Early Detection
Identifying and treating heart failure early amplifies the potential for reversal. Be alert for “red flag” symptoms:
• Unexplained fatigue and weakness
• Shortness of breath during routine activities or at rest
• Swelling in legs, ankles, or abdomen
• Persistent cough or wheezing with pink, frothy sputum
Prompt medical evaluation—echocardiogram, blood tests (BNP/NT-proBNP), and specialist referral—can catch the condition when it’s most reversible.
Conclusion
So, is congestive heart failure reversible? The answer lies in shades of gray rather than a simple yes or no. While chronic, irreversible scarring may limit full recovery, many patients achieve meaningful improvements—often referred to as reverse remodeling—through timely, evidence-based treatment and lifestyle changes. Early diagnosis, strict adherence to medications, diet and exercise modifications, and addressing underlying causes all boost the odds. Even if full reversal isn’t possible, modern therapies can transform a heart-failure diagnosis from a life sentence into a manageable condition, empowering you to live more fully. Talk to your cardiologist about building a personalized plan—because when it comes to your heart, every beat (and every decision) counts.











3 Responses