Endometriosis: Understanding a Common but Often Misunderstood Condition
Endometriosis is a chronic medical condition that affects millions of people worldwide, yet it often goes undiagnosed for years. It can significantly impact physical health, quality of life, and emotional well-being. This article provides a clear, medically accurate overview of endometriosis, what it is, why it happens, how it presents, and how it is managed, using accessible language for a general audience.
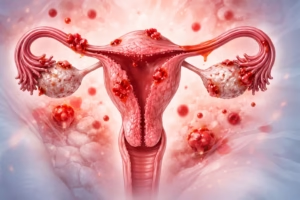
Overview / Definition
Endometriosis is a condition in which tissue similar to the lining of the uterus (called the endometrium) grows outside the uterus. These growths, known as endometriotic lesions, can be found on:
- The ovaries
- Fallopian tubes
- Outer surface of the uterus
- Pelvic ligaments
- Bladder or bowel (less commonly)
Unlike normal uterine lining, which sheds during menstruation, this tissue has no way to exit the body. As a result, it can lead to inflammation, pain, scar tissue (adhesions), and sometimes fertility challenges.
Endometriosis is most commonly diagnosed in individuals of reproductive age, but symptoms can begin during adolescence.
Causes or Risk Factors
The exact cause of endometriosis is not fully understood. Several theories and contributing factors have been proposed, including:
- Retrograde menstruation: Menstrual blood flows backward through the fallopian tubes into the pelvic cavity
- Immune system dysfunction: Reduced ability to clear misplaced endometrial-like tissue
- Hormonal influences: Estrogen appears to promote the growth of endometriotic tissue
- Genetic factors: A family history of endometriosis increases risk
- Cellular transformation: Certain cells may change into endometrial-like cells under specific conditions
Known Risk Factors
- Early onset of menstruation
- Short menstrual cycles
- Heavy or prolonged menstrual bleeding
- Never having given birth
- First-degree relatives with endometriosis
Symptoms or Clinical Presentation
Symptoms vary widely, and the severity of symptoms does not always match the extent of disease. Some individuals have significant disease with few symptoms, while others experience severe pain.
Common Symptoms Include:
- Chronic pelvic pain
- Painful menstrual periods (dysmenorrhea)
- Pain during or after sexual intercourse
- Pain with bowel movements or urination, especially during menstruation
- Heavy menstrual bleeding or bleeding between periods
- Fatigue
- Difficulty conceiving or infertility
Because these symptoms can overlap with other conditions, endometriosis is often misattributed to “normal” menstrual pain, leading to delayed diagnosis.
Diagnosis or Screening
There is currently no single non-invasive test that definitively diagnoses endometriosis.
Diagnostic Approaches May Include:
- Clinical evaluation: Detailed medical history and pelvic examination
- Imaging studies: Ultrasound or MRI may identify cysts such as endometriomas, but smaller lesions can be missed
- Laparoscopy: A minimally invasive surgical procedure considered the gold standard for diagnosis, allowing direct visualization and biopsy
Diagnosis may take several years from the onset of symptoms, emphasizing the need for awareness and early evaluation.
Treatment or Management Options
There is no cure for endometriosis, but symptoms can often be effectively managed. Treatment is individualized and depends on symptom severity, age, and reproductive goals.
Common Management Strategies:
- Pain management: Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Hormonal therapies:
- Combined oral contraceptives
- Progestins
- Gonadotropin-releasing hormone (GnRH) analogs
- Surgical treatment:
- Laparoscopic removal or destruction of endometriotic lesions
- Surgery may improve pain and fertility outcomes in selected cases
A multidisciplinary approach involving gynecologists, pain specialists, and mental health professionals is often beneficial for long-term management.
Prevention or Lifestyle Considerations
There is no proven way to prevent endometriosis, but certain lifestyle strategies may help support symptom management:
- Regular physical activity
- Balanced, anti-inflammatory dietary patterns
- Stress reduction techniques (e.g., mindfulness, counseling)
- Adequate sleep
- Avoiding smoking, which may worsen inflammation
Lifestyle measures are best viewed as complementary to, not replacements for, medical care.
Conclusion: Key Takeaways
Endometriosis is a common, chronic condition that can have profound effects on health and daily life. Key points to remember include:
- It involves the growth of endometrial-like tissue outside the uterus
- Symptoms vary widely and may include pain, heavy periods, and infertility
- Diagnosis often takes time and may require surgical confirmation
- Treatment focuses on symptom control and quality of life, using medical and surgical options
Increased awareness, early recognition of symptoms, and access to appropriate care are essential in improving outcomes for those affected.
Medical Disclaimer
This article is intended for educational purposes only and does not replace professional medical advice. Individuals experiencing symptoms or concerns related to endometriosis should consult a qualified healthcare professional for personalized evaluation and care.






