Blood Clots: What You Need to Know for Better Health
Blood clots are a natural and essential part of the body’s healing process, but when they form at the wrong time or in the wrong place, they can become serious and even life-threatening. Understanding how blood clots develop, recognizing warning signs, and knowing how they are managed can help individuals make informed decisions and seek timely medical care.
This article provides a clear, medically accurate overview of blood clots, written in accessible language for a general audience.
Overview: What Are Blood Clots?
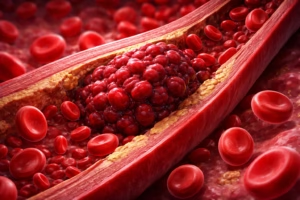
A blood clot (also called a thrombus) is a gel-like collection of blood cells and proteins that forms to stop bleeding when a blood vessel is injured. Under normal circumstances, this process—known as coagulation, protects the body from excessive blood loss.
Problems arise when blood clots:
- Form without an obvious injury
- Grow too large
- Block normal blood flow
- Travel to vital organs such as the lungs or brain
Depending on where a clot forms, it may lead to conditions such as:
- Deep vein thrombosis (DVT) – clots in deep veins, often in the legs
- Pulmonary embolism (PE) – a clot that travels to the lungs
- Stroke – a clot blocking blood flow to the brain
- Heart attack – clots affecting coronary arteries
Causes and Risk Factors
Blood clots often develop due to a combination of factors affecting blood flow, vessel walls, or clotting behavior, sometimes referred to as Virchow’s triad.
Common risk factors include:
- Prolonged immobility
- Long hospital stays
- Extended bed rest
- Long-distance travel
- Surgery or trauma, especially orthopedic procedures
- Certain medical conditions
- Cancer
- Heart disease
- Autoimmune disorders
- Hormonal factors
- Pregnancy
- Oral contraceptives or hormone replacement therapy
- Lifestyle factors
- Smoking
- Obesity
- Dehydration
- Inherited clotting disorders
- Such as Factor V Leiden mutation
Having one or more risk factors does not guarantee a blood clot will form, but it does increase the likelihood.
Symptoms and Clinical Presentation
Symptoms of blood clots vary depending on their location and severity. Some clots may cause no noticeable symptoms, while others require emergency attention.
Common signs of deep vein thrombosis (DVT):
- Swelling in one leg or arm
- Pain or tenderness, often described as cramping
- Warmth or redness over the affected area
Signs of a pulmonary embolism (medical emergency):
- Sudden shortness of breath
- Chest pain that worsens with deep breathing
- Rapid heartbeat
- Coughing, sometimes with blood
Signs associated with stroke or heart attack:
- Sudden weakness or numbness on one side of the body
- Difficulty speaking or understanding speech
- Severe headache
- Chest pressure or pain radiating to the arm or jaw
Diagnosis and Screening
Diagnosing a blood clot typically involves a combination of clinical evaluation and imaging tests.
Common diagnostic tools include:
- Ultrasound – often used to detect DVT in the legs
- CT pulmonary angiography – to identify pulmonary embolisms
- MRI or CT scans – for clots in the brain or other organs
- Blood tests
- D-dimer tests may indicate abnormal clot formation but are not definitive
Screening is usually considered for individuals with significant risk factors or symptoms rather than the general population.
Treatment and Management Options
Treatment aims to prevent the clot from growing, reduce the risk of new clots, and minimize complications.
Common medical approaches:
- Anticoagulant medications (“blood thinners”)
- Reduce the blood’s ability to clot
- Examples include heparin, warfarin, and newer oral anticoagulants
- Thrombolytic therapy
- Medications that dissolve clots in severe, life-threatening cases
- Mechanical interventions
- Catheter-based clot removal
- Inferior vena cava (IVC) filters to prevent clots from reaching the lungs
The choice and duration of treatment depend on the clot’s location, underlying cause, and overall health status.
Prevention and Lifestyle Considerations
While not all blood clots are preventable, certain measures may reduce risk—especially for individuals with known risk factors.
Evidence-based prevention strategies include:
- Staying physically active and avoiding prolonged immobility
- Maintaining a healthy weight
- Staying well hydrated
- Avoiding tobacco use
- Following movement recommendations during long travel
- Using prescribed preventive medications when recommended by healthcare providers
Prevention plans are often tailored based on individual risk profiles.
Conclusion: Key Takeaways About Blood Clots
Blood clots play a vital role in healing, but abnormal clot formation can pose serious health risks. Recognizing common risk factors, understanding warning symptoms, and being aware of diagnostic and treatment options can support timely medical evaluation. Advances in medical care have significantly improved outcomes, especially when clots are identified early.
Medical Disclaimer
This article is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. If you have concerns about blood clots or related symptoms, consult a qualified healthcare professional for personalized guidance.






