Introduction
Living with diabetes already requires diligent monitoring, blood sugar checks, dietary adjustments, and regular medical visits. When hypertension enters the picture, the stakes rise even higher. High blood pressure not only accelerates diabetic complications like nephropathy and retinopathy but also adds complexity to insurance claims and medical records. That’s where accurate ICD-10 coding for hypertension complicating diabetes becomes essential. In this post, we’ll explore why precise code selection matters, review the primary ICD-10 codes you’ll need, and share best practices for documentation and clinical management.
Understanding the Diabetes–Hypertension Connection and ICD-10 Coding
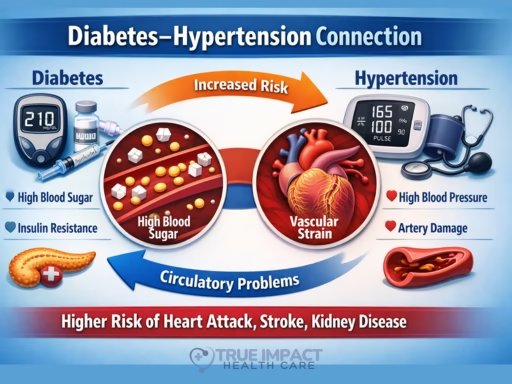
Understanding the Diabetes–Hypertension Connection
Diabetes mellitus (both type 1 and type 2) and hypertension frequently occur together and interact in ways that amplify disease severity. Rather than viewing hypertension as a separate condition, clinicians increasingly regard it as part of a pathophysiological continuum driven by metabolic and vascular dysfunction.
Shared Risk Factors
Several overlapping lifestyle and biological factors predispose individuals to both conditions:
-
Obesity and insulin resistance
Excess adiposity promotes chronic inflammation and impaired glucose metabolism. Insulin resistance — a hallmark of type 2 diabetes — is also commonly observed in people with hypertension. -
Sedentary lifestyle and poor diet
Physical inactivity and diets high in processed foods or added sugars contribute to metabolic syndrome, raising the likelihood of both hyperglycemia and elevated blood pressure.
These shared drivers explain why co-occurrence is so common: epidemiological data show roughly two-thirds of individuals with diabetes also have high blood pressure or take antihypertensive medication.
Vascular Damage and Pathophysiology
The biological interplay between diabetes and hypertension occurs largely at the vascular level:
-
Endothelial injury from hyperglycemia
Persistently elevated blood glucose damages blood vessel walls, making them narrower and less elastic, which contributes to rising blood pressure. -
Insulin resistance and nitric oxide disruption
Metabolic changes associated with high sugar intake and insulin resistance can impair nitric oxide signaling — essential for vessel dilation — resulting in vasoconstriction and increased blood pressure. -
Renal involvement
High blood sugar may harm kidney structures that regulate fluid and electrolyte balance, indirectly elevating blood pressure.
These mechanisms illustrate a feedback loop: diabetes promotes hypertension, and hypertension further worsens vascular and metabolic injury.
Compounded Complications
When both conditions coexist, risks escalate dramatically:
-
Accelerated diabetic nephropathy (kidney disease progression)
-
Increased incidence of cardiovascular events, including heart attack and stroke
-
A substantially higher likelihood of serious cardiovascular outcomes — estimates suggest the combined presence raises heart disease or stroke risk severalfold compared with having neither condition.
Recognizing this synergy allows healthcare teams to prioritize integrated treatment strategies rather than addressing each disorder independently.
Why Accurate ICD-10 Coding Matters
From a clinical documentation and revenue-cycle perspective, coding precision has direct implications beyond administrative classification.
Clinical Clarity
Accurate ICD-10 coding communicates the patient’s full disease burden to multidisciplinary teams. A correctly coded record ensures that cardiologists, endocrinologists, and primary providers immediately recognize comorbid complexity.
Billing Compliance
Coding errors — such as missing linkage between diabetes and hypertension — may result in claim rejections, delayed reimbursement, or compliance audits. Proper specificity protects against revenue leakage.
Quality Reporting and Population Health
Healthcare organizations rely on coded datasets for benchmarking, research, and epidemiological surveillance. Inaccurate coding distorts population-level statistics and quality metrics.
Risk Adjustment and Reimbursement
Many payer models adjust compensation based on patient acuity. Complete coding captures disease severity, enabling fair resource allocation and reimbursement under value-based frameworks.
Key ICD-10 Codes for Hypertension Complicating Diabetes
When coding hypertension in the context of diabetes, documentation must identify:
-
The type or cause of diabetes
-
The presence of hypertension
-
Any target-organ complications
These are typically represented using combination codes in the E08–E13 series, with subclassification indicating hypertensive involvement.
Common Examples
-
E08.22
Diabetes mellitus due to an underlying condition with hypertension -
E09.22
Drug- or chemical-induced diabetes mellitus with hypertension -
E10.22
Type 1 diabetes mellitus with hypertension -
E11.22
Type 2 diabetes mellitus with hypertension -
E13.22
Other specified diabetes mellitus with hypertension
These codes are used alongside additional documentation specifying complications or manifestations if present.
Coding Best Practices
-
Verify specificity
Always review characters beyond the decimal to capture complications such as nephropathy, retinopathy, or neuropathy. -
Consult coding manuals and payer policies
Guidelines may evolve; referencing current coding resources ensures compliance. -
Align documentation with clinical findings
Coding accuracy depends on clear physician notes linking hypertension to diabetes when applicable.
Best Practices for Documentation and Coding
Accurate documentation is the foundation of compliant coding and effective patient management. When diabetes and hypertension coexist, clinical notes must clearly reflect disease complexity, causal relationships, and severity to support appropriate ICD-10 selection and reimbursement.
Detailed History & Physical Examination
A thorough history and examination provide the clinical evidence necessary for both treatment decisions and defensible coding.
-
Blood Pressure Trends
Documentation should reflect longitudinal patterns rather than isolated readings. For example:
“Persistent readings exceeding 130/80 mmHg across two or more visits despite lifestyle modification.”
Include:-
Dates and values of measurements
-
Context (resting vs. ambulatory readings)
-
Medication adherence or recent therapy changes
-
-
Diabetes Characterization
Specify:-
Type of diabetes (Type 1, Type 2, secondary, drug-induced)
-
Duration since diagnosis
-
Recent lab markers (HbA1c, fasting glucose)
-
Evidence of complications such as neuropathy, nephropathy, or retinopathy
-
-
Objective Findings
Incorporate physical exam indicators including:-
BMI or waist circumference
-
Signs of vascular compromise
-
Renal or cardiac findings relevant to comorbidity assessment
-
This level of detail supports risk stratification and ensures coders can assign the highest level of specificity.
Explicit Linkage Between Conditions
Clinical documentation must clearly establish causal or contributory relationships between hypertension and diabetes when applicable.
-
Use Definitive Language
Statements such as:-
“Hypertension secondary to long-standing type 2 diabetes mellitus”
-
“Diabetic nephropathy contributing to elevated blood pressure”
enable coders to select combination codes.
-
-
Avoid Ambiguity
Listing conditions side-by-side (e.g., “HTN, DM”) without clarification forces conservative coding and may reduce reimbursement accuracy or clinical clarity. -
Clarify Non-Relationships
If conditions are unrelated, explicitly state this to prevent incorrect assumptions during coding.
Use Structured Documentation Templates
Standardized templates improve consistency, completeness, and audit readiness.
Include dedicated fields for:
-
Diabetes classification and complications
-
Hypertension stage or severity
-
Evidence of end-organ damage (renal, cardiovascular, ocular)
-
Medication regimens and response
-
Monitoring outcomes
Electronic health record (EHR) templates can guide clinicians toward comprehensive documentation while reducing omissions.
Double-Check Code Compliance
Even with detailed notes, validation is essential.
-
Cross-Reference Official Coding Resources
Compare assigned codes with current ICD-10 manuals and payer-specific policies to ensure alignment with regulatory standards. -
Leverage Coding Tools
Modern coding platforms provide automated validation and alerts for:-
Missing linkage indicators
-
Unsupported specificity
-
Conflicting diagnoses
-
-
Internal Audits
Periodic chart reviews strengthen compliance and identify documentation gaps before external audits occur.
Clinical Implications and Management Strategies
Effective care extends beyond administrative accuracy. Managing concurrent diabetes and hypertension is essential for reducing morbidity and preventing long-term complications.
Lifestyle Modifications
Behavioral interventions form the cornerstone of risk reduction.
-
Dietary Optimization
The DASH (Dietary Approaches to Stop Hypertension) framework emphasizes:-
Fruits and vegetables rich in potassium
-
Whole grains and lean proteins
-
Reduced sodium intake
For diabetic patients, this overlaps with glycemic control strategies, supporting dual benefits.
-
-
Physical Activity
At least 150 minutes of moderate aerobic activity weekly improves insulin sensitivity, aids weight control, and lowers blood pressure. -
Weight Management
Even modest weight reduction can significantly improve metabolic and cardiovascular parameters.
Pharmacological Therapy
Medication strategies should target both metabolic and vascular protection.
-
Antihypertensives
ACE inhibitors or ARBs are often first-line due to renal protective effects in diabetic patients. Additional agents may be layered depending on response and comorbidity profile. -
Antidiabetic Therapy
-
Metformin commonly serves as foundational therapy for type 2 diabetes
-
Treatment intensification may include additional agents based on glycemic targets
-
-
Polypharmacy Coordination
Medication reconciliation is essential to prevent interactions and ensure adherence.
Monitoring and Follow-Up
Ongoing surveillance allows early detection of deterioration or complications.
-
Laboratory Monitoring
-
HbA1c approximately every three months
-
Lipid panels semiannually or as clinically indicated
-
-
Home Blood Pressure Tracking
Encouraging patients to maintain logs supports:-
Treatment adjustments
-
Detection of white-coat or masked hypertension
-
-
Routine Clinical Reviews
Regular reassessment helps refine therapy and documentation accuracy.
Patient Education
Empowering patients improves outcomes and adherence.
-
Emergency Awareness
Patients should recognize warning signs such as severe headaches, chest pain, or vision changes that may signal hypertensive crisis. -
Self-Management Skills
Instruction on:-
Carbohydrate counting
-
Medication timing
-
Understanding interactions between glucose levels and blood pressure
-
-
Engagement in Care Plans
Collaborative goal setting promotes long-term compliance and health literacy.
Conclusion
Hypertension complicating diabetes isn’t just a clinical challenge—it’s a coding and documentation imperative. By mastering the ICD-10 codes specific to this dual diagnosis, healthcare professionals can ensure accurate billing, support high-quality patient care, and contribute valuable data to population health initiatives. Remember: precise documentation is the foundation for effective treatment plans, optimal reimbursement, and improved patient outcomes. Start implementing these best practices today, and take your diabetes-hypertension management to the next level.